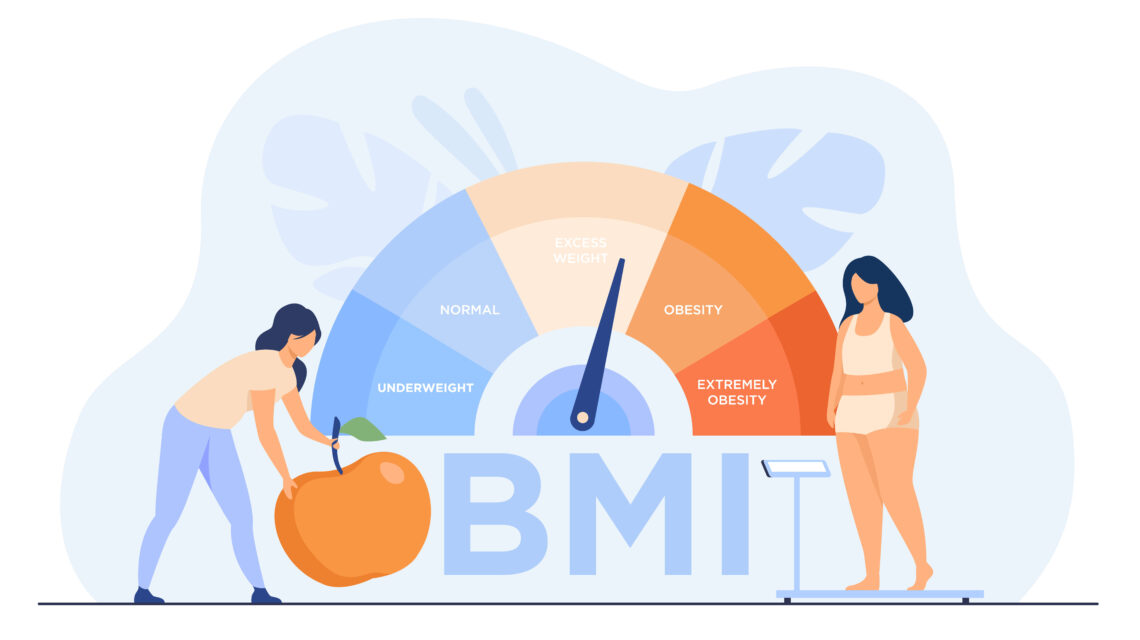
Bariatric surgery is a significant medical intervention aimed at facilitating considerable and lasting weight reduction for those grappling with extreme obesity. Although it presents a viable solution, the procedure is not universally applicable. Understanding who qualifies for bariatric surgery involves a detailed assessment of eligibility criteria, encompassing a range of determinants such as body mass index (BMI), the presence of obesity-related health issues, psychological readiness, age restrictions, and the history of prior endeavors to lose weight.
BMI Requirements for Bariatric Surgery

The specific BMI thresholds for qualifying for bariatric surgery may vary depending on the guidelines set by different medical organizations and healthcare providers. However, I can provide you with a general overview of commonly used BMI thresholds:
Body Mass Index (BMI)
BMI is a measurement that assesses an individual’s body fat based on their height and weight. The formula for calculating BMI is weight in kilograms divided by the square of height in meters (BMI = weight / height^2). BMI is categorized into different ranges to determine weight status.
BMI Thresholds for Bariatric Surgery
Generally, bariatric surgery is considered for individuals with a BMI of 40 or higher (known as morbid obesity) or a BMI of 35 or higher with obesity-related health conditions. These thresholds are often used as guidelines to identify candidates who may benefit the most from surgical weight loss interventions.
It’s important to note that these thresholds are not set in stone, and individual patient factors, such as overall health, medical history, and other considerations, are also taken into account during the evaluation process.
Exceptions to BMI Criteria
In some cases, individuals with a BMI below the traditional thresholds may still be considered for bariatric surgery if they have significant obesity-related health conditions that greatly impact their quality of life or pose a significant health risk. This decision is usually made on a case-by-case basis after a thorough evaluation by a healthcare professional.
It’s worth noting that these BMI thresholds may differ based on specific bariatric surgery procedures, such as gastric bypass, sleeve gastrectomy, or gastric banding. The eligibility criteria and BMI thresholds can vary depending on the surgical technique and the guidelines followed by the healthcare provider or institution. Therefore, it is essential to consult with a qualified healthcare professional or bariatric surgeon who can provide accurate and personalized information based on your specific circumstances.
How BMI is Calculated
There are two ways to calculate your Body Mass Index (BMI), depending on which measurement system you’re comfortable with:
Metric Units (kilograms and meters)
- Square your height in meters. For example, if you are 1.7 meters tall, then 1.7 multiplied by itself is 2.89 meters squared.
- Divide your weight in kilograms by the result from step 1. Let’s say you weigh 70 kilograms. Dividing 70 kg by 2.89 meters squared equals 24.22 (round to two decimal places).
Imperial Units (Pounds and Inches)
- Multiply your weight in pounds by 703. If you weigh 180 pounds, then 180 pounds multiplied by 703 is 126,540.
- Divide the result from step 1 by your height in inches squared. Let’s say your height is 5 feet 10 inches, which is 70 inches total (5 feet x 12 inches/foot + 10 inches). So, 70 inches squared is 4,900 inches squared. Divide 126,540 by 4,900, and you get 25.8 (round to two decimal places).
Here’s an interpretation of your BMI:
- Below 18.5: Underweight
- 18.5 to 24.9: Healthy weight
- 25 to 29.9: Overweight
- 30 or above: Obese
Important to Note:
- BMI is a general guideline and may not apply to everyone, particularly for children, pregnant women, or people with a very muscular build.
- It’s always best to consult with a healthcare professional to discuss your weight and overall health. They can consider your BMI along with other factors to determine if you’re a good candidate for weight loss strategies, including bariatric surgery.
Understanding Who Qualifies for Bariatric Surgery
Bariatric surgery, also known as weight-loss surgery, is a powerful tool for individuals struggling with severe obesity. However, it’s not a one-size-fits-all solution, and specific criteria determine eligibility. Here’s a breakdown of the key factors that influence who qualifies for bariatric surgery:
Body Mass Index (BMI): A Starting Point, Not the Finish Line
Body Mass Index (BMI) is a common measurement used to assess weight relative to height. It’s calculated by dividing your weight in kilograms by the square of your height in meters. While BMI is a starting point in determining eligibility for bariatric surgery, it’s not the sole factor. Here’s how BMI is generally considered:
- BMI 40 or higher: Generally considered the primary threshold for surgery.
- BMI 35 to 39.9: May be eligible if you have at least one obesity-related health condition, such as type 2 diabetes, sleep apnea, or severe joint pain.
Important to Note:
- BMI may not be entirely accurate for everyone, particularly for people with very muscular builds or pregnant women.
- Muscle tissue is denser than fat, so someone with a high amount of muscle mass might have a high BMI despite not having excess body fat.
General Criteria for Bariatric Surgery Candidates
Beyond BMI, several additional factors are considered when evaluating candidacy for bariatric surgery:
- Age: Most programs require patients to be between 18 and 65 years old. This ensures individuals are mature enough to understand the commitment required and have a longer lifespan to benefit from the surgery’s long-term effects.
- Weight History: A documented history of attempts at weight loss through diet and exercise programs under medical supervision demonstrates a commitment to healthy habits before considering surgery.
- Overall Health: A thorough evaluation by a healthcare team assesses your overall health and identifies any potential risks associated with surgery.
Medical Conditions Impacted by Obesity
Bariatric surgery can be a viable option for individuals with severe obesity and one or more obesity-related health conditions that significantly impact their quality of life. These conditions may include:
- Type 2 Diabetes: Bariatric surgery can significantly improve blood sugar control and potentially eliminate the need for diabetes medication in some cases.
- Sleep Apnea: Excessive weight can contribute to sleep apnea, a condition where breathing repeatedly stops and starts during sleep. Bariatric surgery can lead to significant improvement in sleep quality.
- Severe Joint Pain: Carrying excess weight puts a strain on your joints, contributing to pain and reduced mobility. Significant weight loss through surgery can significantly reduce joint pain and improve mobility.
- Heart Disease: Obesity is a major risk factor for heart disease. Bariatric surgery can lead to improvements in blood pressure, cholesterol levels, and overall cardiovascular health.
- Non-alcoholic Fatty Liver Disease (NAFLD): This condition can develop due to excess fat buildup in the liver. Bariatric surgery can improve liver function and potentially reverse NAFLD.
The Importance of Psychological Evaluation
Bariatric surgery is a significant life change. A psychological evaluation is typically performed to ensure you have realistic expectations about the surgery and the ongoing lifestyle changes necessary for long-term success. The evaluation may also explore:
- Your motivation for seeking weight-loss surgery
- Your understanding of the risks and benefits of the surgery
- Your ability to commit to the post-surgical dietary and exercise program
- Any underlying emotional factors that may contribute to weight management challenges
Remember: Bariatric surgery is a joint decision between you and your healthcare team. Open communication and a thorough evaluation help determine if you’re a good candidate for the surgery and ensure you have the necessary support system for long-term success.
Understanding BMI and Weight Loss Surgery Options
Body Mass Index (BMI) plays a crucial role in determining eligibility for weight loss procedures. However, BMI is just one piece of the puzzle. This section dives deeper into the relationship between BMI and various aspects of bariatric surgery:
A Spectrum of Surgical Solutions: Matching BMI with the Right Option
Bariatric surgery isn’t a one-size-fits-all solution. Different procedures offer varying levels of weight loss and have suitability ranges based on BMI. Here’s a breakdown of some common bariatric surgeries and their potential BMI considerations:
- Laparoscopic Adjustable Gastric Band (LAGB): This procedure creates an adjustable stomach pouch, restricting food intake. It’s generally suitable for a broader BMI range (30-40) and can be adjusted over time.
- Sleeve Gastrectomy: This surgery removes a portion of the stomach, resulting in a banana-shaped stomach pouch. It’s typically considered for individuals with a BMI of 35 or higher and may lead to faster initial weight loss compared to LAGB.
- Biliopancreatic Diversion with Duodenal Switch (BPD-DS): This surgery involves bypassing a portion of the small intestine, restricting nutrient absorption. It’s usually recommended for individuals with a very high BMI (over 40 or 45) who haven’t achieved sufficient weight loss with other methods due to its more complex nature.
Important to Note:
- These are general guidelines, and your surgeon will determine the best option based on your individual health profile and BMI.
- Newer and less invasive bariatric procedures, such as mini gastric sleeve and mini gastric plication, are constantly evolving, offering additional options for different BMI ranges.
BMI and Success Rates: Understanding the Correlation
Studies suggest a positive correlation between pre-surgical BMI and long-term weight loss success rates after bariatric surgery [1]. Here’s a simplified breakdown:
Individuals with a higher pre-surgical BMI (often above 40) tend to experience more significant initial weight loss percentages. This can be motivating and lead to better long-term adherence to dietary and exercise changes.
However, it’s important to remember that the ultimate goal is sustainable weight loss and overall health improvement. Bariatric surgery offers a powerful tool for individuals with severe obesity, regardless of their specific BMI within the eligible range.
Focusing on the Positive Outcomes
Research shows that bariatric surgery can significantly improve health markers, even for individuals with a lower pre-surgical BMI, particularly those with obesity-related health conditions. Here are some success stories to consider:
- A study found that 80% of patients with type 2 diabetes achieved remission or significant improvement in blood sugar control after bariatric surgery, even with a pre-surgical BMI as low as 30.
- Individuals with severe sleep apnea often experience significant improvement in sleep quality and a reduction in daytime sleepiness after bariatric surgery, regardless of their specific pre-surgical BMI.
The bottom line is that bariatric surgery goes beyond BMI! While a BMI of 35+ is typical, weight history, overall health, and specific conditions like diabetes all play a role. Even with a lower BMI, surgery can improve health. Talk to your doctor to see if it’s right for you.